pulmonary embolism بالتفصيل
3 مشترك
صفحة 1 من اصل 1
 pulmonary embolism بالتفصيل
pulmonary embolism بالتفصيل
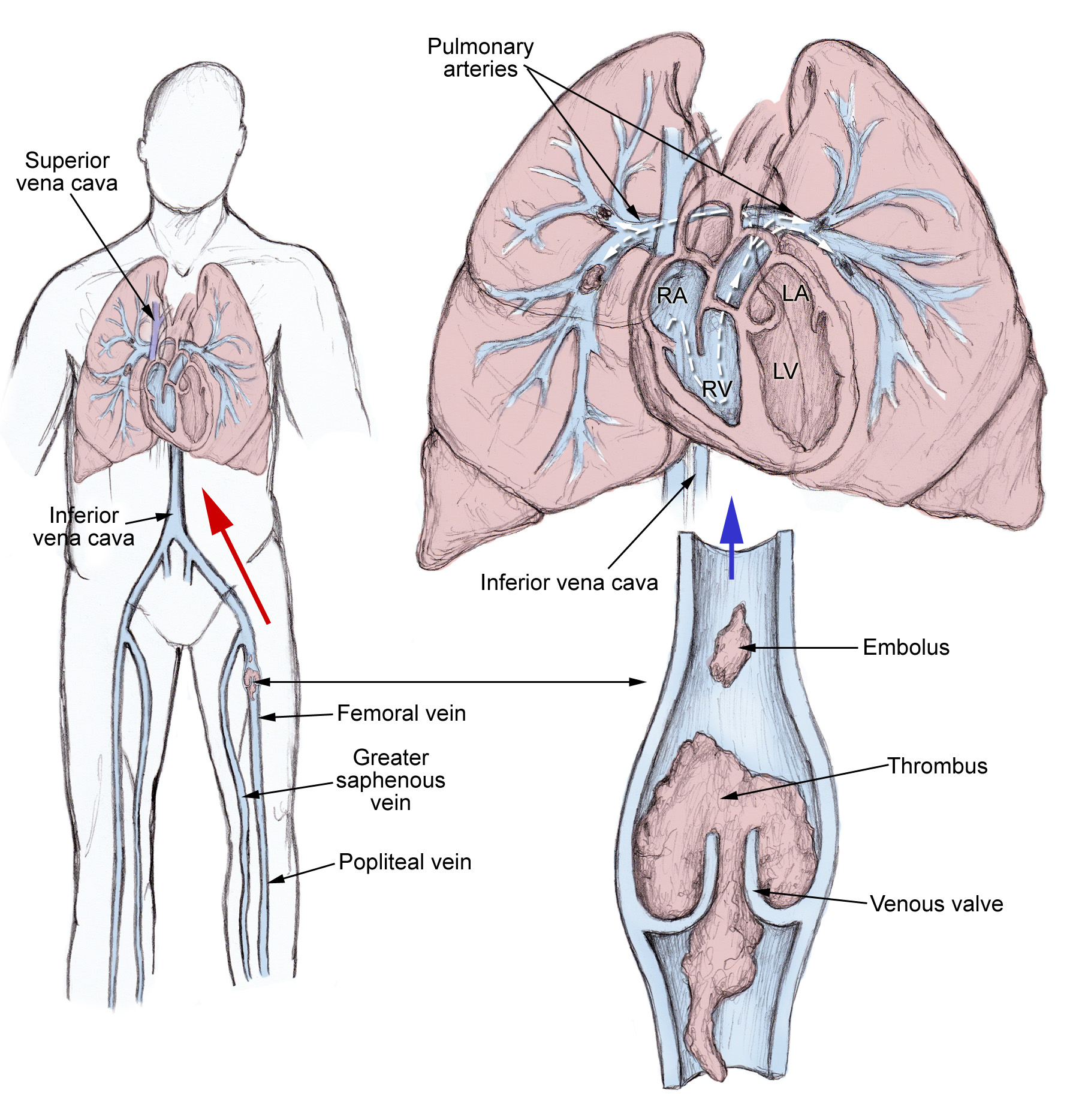
Pulmonary embolism (PE) is a blockage of the main artery of the lung or one of its branches by a substance that has travelled from elsewhere in the body through the bloodstream (embolism). Usually this is due to embolism of a thrombus (blood clot) from the deep veins in the legs, a process termed venous thromboembolism. A small proportion is due to the embolization of air, fat or amniotic fluid. The obstruction of the blood flow through the lungs and the resultant pressure on the right ventricle of the heart leads to the symptoms and signs of PE. The risk of PE is increased in various situations, such as cancer and prolonged bed rest.[1]
Symptoms of pulmonary embolism include difficulty breathing, chest pain on inspiration, and palpitations. Clinical signs include low blood oxygen saturation and cyanosis, rapid breathing, and a rapid heart rate. Severe cases of PE can lead to collapse, abnormally low blood pressure, and sudden death.[1]
Diagnosis is based on these clinical findings in combination with laboratory tests (such as the D-dimer test) and imaging studies, usually CT pulmonary angiography. Treatment is typically with anticoagulant medication, including heparin and warfarin. Severe cases may require thrombolysis with drugs such as tissue plasminogen activator (tPA) or may require surgical intervention via pulmonary thrombectomy.[1
[edit] Signs and symptoms
Symptoms of PE are sudden-onset dyspnea (shortness of breath), tachypnea (rapid breathing), chest pain of a "pleuritic" nature (worsened by breathing), cough and hemoptysis (coughing up blood). More severe cases can include signs such as cyanosis (blue discoloration, usually of the lips and fingers), collapse, and circulatory instability. About 15% of all cases of sudden death are attributable to PE.[sup][1]
On physical examination, a pleural rub may be audible by stethoscope over affected areas of the lung. Strain on the right ventricle may be detected as a left parasternal heave, a loud pulmonary component of the second heart sound, raised jugular venous pressure, and more rarely leg swelling.[1]
A fever though usually low grade is present in 14% of people with pulmonary embolism.[2]
[edit] Diagnosis
The diagnosis of PE is based primarily on validated clinical criteria combined with selective testing because the typical clinical presentation (shortness of breath, chest pain) cannot be definitively differentiated from other causes of chest pain and shortness of breath. The decision to do medical imaging is usually based on clinical grounds, i.e. the medical history, symptoms and findings on physical examination, followed by an assessment of clinical probability.[1]
The most commonly used method to predict clinical probability, the Wells score, is a clinical prediction rule, whose use is complicated by multiple versions being available. In 1995, Wells et al. initially developed a prediction rule (based on a literature search) to predict the likelihood of PE, based on clinical criteria.[3] The prediction rule was revised in 1998[4] This prediction rule was further revised when simplified during a validation by Wells et al. in 2000.[5] In the 2000 publication, Wells proposed two different scoring systems using cutoffs of 2 or 4 with the same prediction rule.[5] In 2001, Wells published results using the more conservative cutoff of 2 to create three categories.[6] An additional version, the "modified extended version", using the more recent cutoff of 2 but including findings from Wells's initial studies[3][4] were proposed.[7] Most recently, a further study reverted to Wells's earlier use of a cutoff of 4 points[5] to create only two categories.[8]
There are additional prediction rules for PE, such as the Geneva rule. More importantly, the use of any rule is associated with reduction in recurrent thromboembolism.[9]
The Wells score:[10]
Traditional interpretation[5][6][11]
Alternate interpretation[5][8]
[edit] Blood tests
In low/moderate suspicion of PE, a normal D-dimer level (shown in a blood test) is enough to exclude the possibility of thrombotic PE.[13]
When a PE is being suspected, a number of blood tests are done, in order to exclude important secondary causes of PE. This includes a full blood count, clotting status (PT, APTT, TT), and some screening tests (erythrocyte sedimentation rate, renal function, liver enzymes, electrolytes). If one of these is abnormal, further investigations might be warranted.
[edit] Medical imaging
The gold standard for diagnosing pulmonary embolism (PE) is pulmonary angiography. Pulmonary angiography is used less often due to wider acceptance of CT scans, which are non-invasive.
Non-invasive imaging
CT pulmonary angiography (CTPA) is a pulmonary angiogram obtained using computed tomography (CT) with radiocontrast rather than right heart catheterization. Its advantages are clinical equivalence, its non-invasive nature, its greater availability to patients, and the possibility of identifying other lung disorders from the differential diagnosis in case there is no pulmonary embolism. Assessing the accuracy of CT pulmonary angiography is hindered by the rapid changes in the number of rows of detectors available in multidetector CT (MDCT) machines.[14] A study with a mixture of 4 slice and 16 slice scanners reported a sensitivity of 83% and a specificity of 96%. This study noted that additional testing is necessary when the clinical probability is inconsistent with the imaging results.[15] CTPA is non-inferior to VQ scanning, and identifies more emboli (without necessarily improving the outcome) compared to VQ scanning.[16]
Ventilation/perfusion scan (or V/Q scan or lung scintigraphy), which shows that some areas of the lung are being ventilated but not perfused with blood (due to obstruction by a clot). This type of examination is used less often because of the more widespread availability of CT technology, however, it may be useful in patients who have an allergy to iodinated contrast or in pregnancy due to lower radiation exposure than CT.[17]
Low probability diagnostic tests/non-diagnostic tests
Tests that are frequently done that are not sensitive for PE, but can be diagnostic.
[edit] Electrocardiogram findings
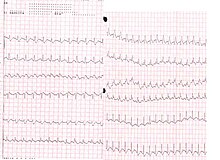
Electrocardiogram of a patient with pulmonary embolism showing sinus tachycardia of approximately 150 beats per minute and right bundle branch block.
An electrocardiogram (ECG) is routinely done on patients with chest pain to quickly diagnose myocardial infarctions (heart attacks). An ECG may show signs of right heart strain or acute cor pulmonale in cases of large PEs - the classic signs are a large S wave in lead I, a large Q wave in lead III and an inverted T wave in lead III ("S1Q3T3").[19] This is occasionally (up to 20%) present, but may also occur in other acute lung conditions and has therefore limited diagnostic value. The most commonly seen signs in the ECG is sinus tachycardia, right axis deviation and right bundle branch block.[20] Sinus tachycardia was however still only found in 8 - 69% of people with PE.[21]
[edit] Echocardiography findings
In massive and submassive PE, dysfunction of the right side of the heart can be seen on echocardiography, an indication that the pulmonary artery is severely obstructed and the heart is unable to match the pressure. Some studies (see below) suggest that this finding may be an indication for thrombolysis. Not every patient with a (suspected) pulmonary embolism requires an echocardiogram, but elevations in cardiac troponins or brain natriuretic peptide may indicate heart strain and warrant an echocardiogram.[22]
The specific appearance of the right ventricle on echocardiography is referred to as the McConnell sign. This is the finding of akinesia of the mid-free wall but normal motion of the apex. This phenomenon has a 77% sensitivity and a 94% specificity for the diagnosis of acute pulmonary embolism.[23]
[edit] Combining tests into algorithms
Recent recommendations for a diagnostic algorithm have been published by the PIOPED investigators; however, these recommendations do not reflect research using 64 slice MDCT.[12] These investigators recommended:
[edit] Pulmonary Embolism Rule-out Criteria
The Pulmonary Embolism Rule-out Criteria, or PERC rule, helps assess patients in whom pulmonary embolism is suspected, but unlikely. Unlike the Wells Score and Geneva score, which are clinical prediction rules intended to risk stratify patients with suspected PE, the PERC rule is designed to rule-out risk of PE in patients when the physician has already stratified them into a low-risk category.
Patients in this low risk category without any of these criteria may undergo no further diagnostic testing for PE: Hypoxia - Sa02 <95%, unilateral leg swelling, hemoptysis, prior DVT or PE, recent surgery or trauma, age >50, hormone use, tachycardia. The rationale behind this decision is that further testing (specifically CT angiogram of the chest) may cause more harm (from radiation exposure and contrast dye) than the risk of PE.[24] The PERC rule has a sensitivity of 97.4% and specificity of 21.9% with a false negative rate of 1.0% (16/1666).[25]
[edit] Treatment
In most cases, anticoagulant therapy is the mainstay of treatment. Acutely, supportive treatments, such as oxygen or analgesia, are often required.
[edit] Anticoagulation
Main article: anticoagulant
In most cases, anticoagulant therapy is the mainstay of treatment. Heparin, low molecular weight heparins (such as enoxaparin and dalteparin), or fondaparinux is administered initially, while warfarin, acenocoumarol, or phenprocoumon therapy is commenced (this may take several days, usually while the patient is in hospital). It however may be possible to treat low risk patients as outpatients.[26] An ongoing study is looking into the safety of this practice.[27] Warfarin therapy often requires frequent dose adjustment and monitoring of the INR. In PE, INRs between 2.0 and 3.0 are generally considered ideal. If another episode of PE occurs under warfarin treatment, the INR window may be increased to e.g. 2.5-3.5 (unless there are contraindications) or anticoagulation may be changed to a different anticoagulant e.g. low molecular weight heparin. In patients with an underlying malignancy, therapy with a course of low molecular weight heparin may be favored over warfarin based on the results of the CLOT trial.[28] Similarly, pregnant women are often maintained on low molecular weight heparin to avoid the known teratogenic effects of warfarin, especially in the early stages of pregnancy. People are usually admitted to hospital in the early stages of treatment, and tend to remain under inpatient care until INR has reached therapeutic levels. Increasingly, low-risk cases are managed on an outpatient basis in a fashion already common in the treatment of DVT.[29]
Warfarin therapy is usually continued for 3–6 months, or "lifelong" if there have been previous DVTs or PEs, or none of the usual risk factors is present. An abnormal D-dimer level at the end of treatment might signal the need for continued treatment among patients with a first unprovoked pulmonary embolus.[30]
[edit] Thrombolysis
Main article: Thrombolysis
Massive PE causing hemodynamic instability (shock and/or hypotension, defined as a systolic blood pressure <90 mmHg or a pressure drop of 40 mmHg for>15 min if not caused by new-onset arrhythmia, hypovolemia or sepsis) is an indication for thrombolysis, the enzymatic destruction of the clot with medication. It is the best available medical treatment in this situation and is supported by clinical guidelines.[31][32][33]
The use of thrombolysis in non-massive PEs is still debated. The aim of the therapy is to dissolve the clot, but there is an attendant risk of bleeding or stroke.[34] The main indication for thrombolysis is in submassive PE where right ventricular dysfunction can be demonstrated on echocardiography, and the presence of visible thrombus in the atrium.[35]
[edit] Surgical management

Used inferior vena cava filter.
Surgical management of acute pulmonary embolism (pulmonary thrombectomy) is uncommon and has largely been abandoned because of poor long-term outcomes. However, recently, it has gone through a resurgence with the revision of the surgical technique and is thought to benefit selected patients.[36]
Chronic pulmonary embolism leading to pulmonary hypertension (known as chronic thromboembolic hypertension) is treated with a surgical procedure known as a pulmonary thromboendarterectomy.
[edit] Inferior vena cava filter
Main article: inferior vena cava filter
If anticoagulant therapy is contraindicated and/or ineffective, or to prevent new emboli from entering the pulmonary artery and combining with an existing blockage, an inferior vena cava filter may be implanted.[37]
[edit] Risk factors
The most common sources of embolism are proximal leg deep venous thrombosis (DVTs) or pelvic vein thromboses. Any risk factor for DVT also increases the risk that the venous clot will dislodge and migrate to the lung circulation, which happens in up to 15% of all DVTs. The conditions are generally regarded as a continuum termed venous thromboembolism (VTE).
The development of thrombosis is classically due to a group of causes named Virchow's triad (alterations in blood flow, factors in the vessel wall and factors affecting the properties of the blood). Often, more than one risk factor is present.
[/sup]
Pathophysiology
Pulmonary thromboembolism is not a disease in and of itself. Rather, it is a complication of underlying venous thrombosis. Under normal conditions, microthrombi (tiny aggregates of red cells, platelets, and fibrin) are formed and lysed continually within the venous circulatory system. This dynamic equilibrium ensures local hemostasis in response to injury without permitting uncontrolled propagation of clot. Under pathological conditions, microthrombi may escape the normal fibrinolytic system to grow and propagate. Pulmonary embolism (PE) occurs when these propagating clots break loose and embolize to block pulmonary blood vessels.
Thrombosis in the veins is triggered by venostasis, hypercoagulability, and vessel wall inflammation. These 3 underlying causes are known as the Virchow triad. All known clinical risk factors for DVT and PE have their basis in one or more elements of the triad.
Patients who have undergone gynecologic surgery, those with major trauma, and those with indwelling venous catheters may have DVTs that start in an area related to their pathology. For other patients, venous thrombosis most often involves the lower extremities and nearly always starts in the calf veins, which are involved in virtually all cases of symptomatic spontaneous lower extremity DVT. Although DVT starts in the calf veins, in cases of pulmonary embolism, it will usually propagate proximally to the popliteal vessels, and from that area embolize.
Causes
As stated in the Pathophysiology section, the etiology of venous thrombosis and subsequent thromboembolism results from a distortion in Virchow's triad by venostasis, hypercoagulability, or vessel wall inflammation. These risk factors for venous thrombosis and pulmonary embolism can be broken down into hereditary factors and acquired factors.
Acquired factors (The most important clinically identifiable risk factors for DVT and PE are a prior history of DVT or PE, recent surgery or pregnancy, prolonged immobilization, or underlying malignancy.)
Reduced mobility
Fractures
Immobilization
Burns
Obesity
Old age
Malignancy
Chemotherapy
Acute medical illness
AIDS (lupus anticoagulant)
Behçet disease
Congestive heart failure (CHF)
Myocardial infarction
Polycythemia
Systemic lupus erythematosus
Ulcerative colitis
Trauma/major surgery
Spinal cord injury
Catheters (indwelling venous infusion catheters)
Postoperative
Pregnancy
Postpartum period
Oral contraceptives
Estrogen replacements (high dose only)
Drug abuse (intravenous [IV] drugs)
Drug-induced lupus anticoagulant
Hemolytic anemias
Heparin-associated thrombocytopenia
Homocysteinemia
Homocystinuria
Hyperlipidemias
Phenothiazines
Thrombocytosis
Varicose veins
Venography
Venous pacemakers
Venous stasis
Warfarin (first few days of therapy)
Symptoms of pulmonary embolism include difficulty breathing, chest pain on inspiration, and palpitations. Clinical signs include low blood oxygen saturation and cyanosis, rapid breathing, and a rapid heart rate. Severe cases of PE can lead to collapse, abnormally low blood pressure, and sudden death.[1]
Diagnosis is based on these clinical findings in combination with laboratory tests (such as the D-dimer test) and imaging studies, usually CT pulmonary angiography. Treatment is typically with anticoagulant medication, including heparin and warfarin. Severe cases may require thrombolysis with drugs such as tissue plasminogen activator (tPA) or may require surgical intervention via pulmonary thrombectomy.[1
[edit] Signs and symptoms
Symptoms of PE are sudden-onset dyspnea (shortness of breath), tachypnea (rapid breathing), chest pain of a "pleuritic" nature (worsened by breathing), cough and hemoptysis (coughing up blood). More severe cases can include signs such as cyanosis (blue discoloration, usually of the lips and fingers), collapse, and circulatory instability. About 15% of all cases of sudden death are attributable to PE.[sup][1]
On physical examination, a pleural rub may be audible by stethoscope over affected areas of the lung. Strain on the right ventricle may be detected as a left parasternal heave, a loud pulmonary component of the second heart sound, raised jugular venous pressure, and more rarely leg swelling.[1]
A fever though usually low grade is present in 14% of people with pulmonary embolism.[2]
[edit] Diagnosis
The diagnosis of PE is based primarily on validated clinical criteria combined with selective testing because the typical clinical presentation (shortness of breath, chest pain) cannot be definitively differentiated from other causes of chest pain and shortness of breath. The decision to do medical imaging is usually based on clinical grounds, i.e. the medical history, symptoms and findings on physical examination, followed by an assessment of clinical probability.[1]
The most commonly used method to predict clinical probability, the Wells score, is a clinical prediction rule, whose use is complicated by multiple versions being available. In 1995, Wells et al. initially developed a prediction rule (based on a literature search) to predict the likelihood of PE, based on clinical criteria.[3] The prediction rule was revised in 1998[4] This prediction rule was further revised when simplified during a validation by Wells et al. in 2000.[5] In the 2000 publication, Wells proposed two different scoring systems using cutoffs of 2 or 4 with the same prediction rule.[5] In 2001, Wells published results using the more conservative cutoff of 2 to create three categories.[6] An additional version, the "modified extended version", using the more recent cutoff of 2 but including findings from Wells's initial studies[3][4] were proposed.[7] Most recently, a further study reverted to Wells's earlier use of a cutoff of 4 points[5] to create only two categories.[8]
There are additional prediction rules for PE, such as the Geneva rule. More importantly, the use of any rule is associated with reduction in recurrent thromboembolism.[9]
The Wells score:[10]
- clinically suspected DVT - 3.0 points
- alternative diagnosis is less likely than PE - 3.0 points
- tachycardia - 1.5 points
- immobilization/surgery in previous four weeks - 1.5 points
- history of DVT or PE - 1.5 points
- hemoptysis - 1.0 points
- malignancy (treatment for within 6 months, palliative) - 1.0 points
Traditional interpretation[5][6][11]
- Score >6.0 - High (probability 59% based on pooled data[12])
- Score 2.0 to 6.0 - Moderate (probability 29% based on pooled data[12])
- Score <2.0 - Low (probability 15% based on pooled data[12])
Alternate interpretation[5][8]
- Score > 4 - PE likely. Consider diagnostic imaging.
- Score 4 or less - PE unlikely. Consider D-dimer to rule out PE.
[edit] Blood tests
In low/moderate suspicion of PE, a normal D-dimer level (shown in a blood test) is enough to exclude the possibility of thrombotic PE.[13]
When a PE is being suspected, a number of blood tests are done, in order to exclude important secondary causes of PE. This includes a full blood count, clotting status (PT, APTT, TT), and some screening tests (erythrocyte sedimentation rate, renal function, liver enzymes, electrolytes). If one of these is abnormal, further investigations might be warranted.
[edit] Medical imaging
 |
 CT pulmonary angiography ( |
| |
Non-invasive imaging
CT pulmonary angiography (CTPA) is a pulmonary angiogram obtained using computed tomography (CT) with radiocontrast rather than right heart catheterization. Its advantages are clinical equivalence, its non-invasive nature, its greater availability to patients, and the possibility of identifying other lung disorders from the differential diagnosis in case there is no pulmonary embolism. Assessing the accuracy of CT pulmonary angiography is hindered by the rapid changes in the number of rows of detectors available in multidetector CT (MDCT) machines.[14] A study with a mixture of 4 slice and 16 slice scanners reported a sensitivity of 83% and a specificity of 96%. This study noted that additional testing is necessary when the clinical probability is inconsistent with the imaging results.[15] CTPA is non-inferior to VQ scanning, and identifies more emboli (without necessarily improving the outcome) compared to VQ scanning.[16]
Ventilation/perfusion scan (or V/Q scan or lung scintigraphy), which shows that some areas of the lung are being ventilated but not perfused with blood (due to obstruction by a clot). This type of examination is used less often because of the more widespread availability of CT technology, however, it may be useful in patients who have an allergy to iodinated contrast or in pregnancy due to lower radiation exposure than CT.[17]
Low probability diagnostic tests/non-diagnostic tests
Tests that are frequently done that are not sensitive for PE, but can be diagnostic.
- Chest X-rays are often done on patients with shortness of breath to help rule-out other causes, such as congestive heart failure and rib fracture. Chest X-rays in PE are rarely normal,[18] but usually lack signs that suggest the diagnosis of PE (e.g. Westermark sign, Hampton's hump).
- Ultrasonography of the legs, also known as leg doppler, in search of deep venous thrombosis (DVT). The presence of DVT, as shown on ultrasonography of the legs, is in itself enough to warrant anticoagulation, without requiring the V/Q or spiral CT scans (because of the strong association between DVT and PE). This may be valid approach in pregnancy, in which the other modalities would increase the risk of birth defects in the unborn child. However, a negative scan does not rule out PE, and low-radiation dose scanning may be required if the mother is deemed at high risk of having pulmonary embolism.
[edit] Electrocardiogram findings
Electrocardiogram of a patient with pulmonary embolism showing sinus tachycardia of approximately 150 beats per minute and right bundle branch block.
An electrocardiogram (ECG) is routinely done on patients with chest pain to quickly diagnose myocardial infarctions (heart attacks). An ECG may show signs of right heart strain or acute cor pulmonale in cases of large PEs - the classic signs are a large S wave in lead I, a large Q wave in lead III and an inverted T wave in lead III ("S1Q3T3").[19] This is occasionally (up to 20%) present, but may also occur in other acute lung conditions and has therefore limited diagnostic value. The most commonly seen signs in the ECG is sinus tachycardia, right axis deviation and right bundle branch block.[20] Sinus tachycardia was however still only found in 8 - 69% of people with PE.[21]
[edit] Echocardiography findings
In massive and submassive PE, dysfunction of the right side of the heart can be seen on echocardiography, an indication that the pulmonary artery is severely obstructed and the heart is unable to match the pressure. Some studies (see below) suggest that this finding may be an indication for thrombolysis. Not every patient with a (suspected) pulmonary embolism requires an echocardiogram, but elevations in cardiac troponins or brain natriuretic peptide may indicate heart strain and warrant an echocardiogram.[22]
The specific appearance of the right ventricle on echocardiography is referred to as the McConnell sign. This is the finding of akinesia of the mid-free wall but normal motion of the apex. This phenomenon has a 77% sensitivity and a 94% specificity for the diagnosis of acute pulmonary embolism.[23]
[edit] Combining tests into algorithms
Recent recommendations for a diagnostic algorithm have been published by the PIOPED investigators; however, these recommendations do not reflect research using 64 slice MDCT.[12] These investigators recommended:
- Low clinical probability. If negative D-dimer, PE is excluded. If positive D-dimer, obtain MDCT and based treatment on results.
- Moderate clinical probability. If negative D-dimer, PE is excluded. However, the authors were not concerned that a negative MDCT with negative D-dimer in this setting has an 5% probability of being false. Presumably, the 5% error rate will fall as 64 slice MDCT is more commonly used. If positive D-dimer, obtain MDCT and based treatment on results.
- High clinical probability. Proceed to MDCT. If positive, treat, if negative, additional tests are needed to exclude PE.
[edit] Pulmonary Embolism Rule-out Criteria
The Pulmonary Embolism Rule-out Criteria, or PERC rule, helps assess patients in whom pulmonary embolism is suspected, but unlikely. Unlike the Wells Score and Geneva score, which are clinical prediction rules intended to risk stratify patients with suspected PE, the PERC rule is designed to rule-out risk of PE in patients when the physician has already stratified them into a low-risk category.
Patients in this low risk category without any of these criteria may undergo no further diagnostic testing for PE: Hypoxia - Sa02 <95%, unilateral leg swelling, hemoptysis, prior DVT or PE, recent surgery or trauma, age >50, hormone use, tachycardia. The rationale behind this decision is that further testing (specifically CT angiogram of the chest) may cause more harm (from radiation exposure and contrast dye) than the risk of PE.[24] The PERC rule has a sensitivity of 97.4% and specificity of 21.9% with a false negative rate of 1.0% (16/1666).[25]
[edit] Treatment
In most cases, anticoagulant therapy is the mainstay of treatment. Acutely, supportive treatments, such as oxygen or analgesia, are often required.
[edit] Anticoagulation
Main article: anticoagulant
In most cases, anticoagulant therapy is the mainstay of treatment. Heparin, low molecular weight heparins (such as enoxaparin and dalteparin), or fondaparinux is administered initially, while warfarin, acenocoumarol, or phenprocoumon therapy is commenced (this may take several days, usually while the patient is in hospital). It however may be possible to treat low risk patients as outpatients.[26] An ongoing study is looking into the safety of this practice.[27] Warfarin therapy often requires frequent dose adjustment and monitoring of the INR. In PE, INRs between 2.0 and 3.0 are generally considered ideal. If another episode of PE occurs under warfarin treatment, the INR window may be increased to e.g. 2.5-3.5 (unless there are contraindications) or anticoagulation may be changed to a different anticoagulant e.g. low molecular weight heparin. In patients with an underlying malignancy, therapy with a course of low molecular weight heparin may be favored over warfarin based on the results of the CLOT trial.[28] Similarly, pregnant women are often maintained on low molecular weight heparin to avoid the known teratogenic effects of warfarin, especially in the early stages of pregnancy. People are usually admitted to hospital in the early stages of treatment, and tend to remain under inpatient care until INR has reached therapeutic levels. Increasingly, low-risk cases are managed on an outpatient basis in a fashion already common in the treatment of DVT.[29]
Warfarin therapy is usually continued for 3–6 months, or "lifelong" if there have been previous DVTs or PEs, or none of the usual risk factors is present. An abnormal D-dimer level at the end of treatment might signal the need for continued treatment among patients with a first unprovoked pulmonary embolus.[30]
[edit] Thrombolysis
Main article: Thrombolysis
Massive PE causing hemodynamic instability (shock and/or hypotension, defined as a systolic blood pressure <90 mmHg or a pressure drop of 40 mmHg for>15 min if not caused by new-onset arrhythmia, hypovolemia or sepsis) is an indication for thrombolysis, the enzymatic destruction of the clot with medication. It is the best available medical treatment in this situation and is supported by clinical guidelines.[31][32][33]
The use of thrombolysis in non-massive PEs is still debated. The aim of the therapy is to dissolve the clot, but there is an attendant risk of bleeding or stroke.[34] The main indication for thrombolysis is in submassive PE where right ventricular dysfunction can be demonstrated on echocardiography, and the presence of visible thrombus in the atrium.[35]
[edit] Surgical management

Used inferior vena cava filter.
Surgical management of acute pulmonary embolism (pulmonary thrombectomy) is uncommon and has largely been abandoned because of poor long-term outcomes. However, recently, it has gone through a resurgence with the revision of the surgical technique and is thought to benefit selected patients.[36]
Chronic pulmonary embolism leading to pulmonary hypertension (known as chronic thromboembolic hypertension) is treated with a surgical procedure known as a pulmonary thromboendarterectomy.
[edit] Inferior vena cava filter
Main article: inferior vena cava filter
If anticoagulant therapy is contraindicated and/or ineffective, or to prevent new emboli from entering the pulmonary artery and combining with an existing blockage, an inferior vena cava filter may be implanted.[37]
[edit] Risk factors
The most common sources of embolism are proximal leg deep venous thrombosis (DVTs) or pelvic vein thromboses. Any risk factor for DVT also increases the risk that the venous clot will dislodge and migrate to the lung circulation, which happens in up to 15% of all DVTs. The conditions are generally regarded as a continuum termed venous thromboembolism (VTE).
The development of thrombosis is classically due to a group of causes named Virchow's triad (alterations in blood flow, factors in the vessel wall and factors affecting the properties of the blood). Often, more than one risk factor is present.
- Alterations in blood flow: immobilization (after surgery, injury or long-distance air travel), pregnancy (also procoagulant), obesity (also procoagulant)
- Factors in the vessel wall: of limited direct relevance in VTE
- Factors affecting the properties of the blood (procoagulant state):
- Oestrogen-containing hormonal contraception
- Genetic thrombophilia (factor V Leiden, prothrombin mutation G20210A, protein C deficiency, protein S deficiency, antithrombin deficiency, hyperhomocysteinemia and plasminogen/fibrinolysis disorders).
- Acquired thrombophilia (antiphospholipid syndrome, nephrotic syndrome, paroxysmal nocturnal hemoglobinuria
[/sup]
Pathophysiology
[ CLOSE WINDOW ]
The pathophysiology of pulmonary embolism. Although pulmonary embolism can arise from anywhere in the body, most commonly it arises from the calf veins. The venous thrombi predominately originate in venous valve pockets (inset) and at other sites of presumed venous stasis. To reach the lungs, thromboemboli travel through the right side of the heart. RA, right atrium; RV, right ventricle; LA, left atrium; LV, left ventricle.
The pathophysiology of pulmonary embolism. Although pulmonary embolism can arise from anywhere in the body, most commonly it arises from the calf veins. The venous thrombi predominately originate in venous valve pockets (inset) and at other sites of presumed venous stasis. To reach the lungs, thromboemboli travel through the right side of the heart. RA, right atrium; RV, right ventricle; LA, left atrium; LV, left ventricle.
Pulmonary thromboembolism is not a disease in and of itself. Rather, it is a complication of underlying venous thrombosis. Under normal conditions, microthrombi (tiny aggregates of red cells, platelets, and fibrin) are formed and lysed continually within the venous circulatory system. This dynamic equilibrium ensures local hemostasis in response to injury without permitting uncontrolled propagation of clot. Under pathological conditions, microthrombi may escape the normal fibrinolytic system to grow and propagate. Pulmonary embolism (PE) occurs when these propagating clots break loose and embolize to block pulmonary blood vessels.
Thrombosis in the veins is triggered by venostasis, hypercoagulability, and vessel wall inflammation. These 3 underlying causes are known as the Virchow triad. All known clinical risk factors for DVT and PE have their basis in one or more elements of the triad.
Patients who have undergone gynecologic surgery, those with major trauma, and those with indwelling venous catheters may have DVTs that start in an area related to their pathology. For other patients, venous thrombosis most often involves the lower extremities and nearly always starts in the calf veins, which are involved in virtually all cases of symptomatic spontaneous lower extremity DVT. Although DVT starts in the calf veins, in cases of pulmonary embolism, it will usually propagate proximally to the popliteal vessels, and from that area embolize.
Causes
As stated in the Pathophysiology section, the etiology of venous thrombosis and subsequent thromboembolism results from a distortion in Virchow's triad by venostasis, hypercoagulability, or vessel wall inflammation. These risk factors for venous thrombosis and pulmonary embolism can be broken down into hereditary factors and acquired factors.
- Hereditary factors (most result in a hypercoagulable state)
- Antithrombin III deficiency
- Protein C deficiency
- Protein S deficiency
- Factor V Leiden (most common genetic risk factor for thrombophilia)
- Plasminogen abnormality
- Plasminogen activator abnormality
- Fibrinogen abnormality
- Resistance to activated protein C

سندباد العرب- .

- تاريخ التسجيل : 12/11/2009
 رد: pulmonary embolism بالتفصيل
رد: pulmonary embolism بالتفصيل
بصراحه موضوع جميل جدا
بس لو سمحت انا كنت محتاجه محاضره أو حصيله عن shock وبجد أكون شاكره أفضالكم جدا
لان بصراحه أنا كلية تمريض بور سعيد والدكاتره مش عايزين ينزلو المحاضرات وانا بحاول أدور علي أي حاجه بس صعب لان المواضيع كبيره وكتيره
عموما أكون سعيده جدا لو حد يقدر يساعدني يا جماعه
بجد ألف شكر
بس لو سمحت انا كنت محتاجه محاضره أو حصيله عن shock وبجد أكون شاكره أفضالكم جدا
لان بصراحه أنا كلية تمريض بور سعيد والدكاتره مش عايزين ينزلو المحاضرات وانا بحاول أدور علي أي حاجه بس صعب لان المواضيع كبيره وكتيره
عموما أكون سعيده جدا لو حد يقدر يساعدني يا جماعه
بجد ألف شكر

الاميره- .

- العمر : 33
تاريخ التسجيل : 11/03/2010
صفحة 1 من اصل 1
صلاحيات هذا المنتدى:
لاتستطيع الرد على المواضيع في هذا المنتدى